Stelara Enrollment Form – Download Patient Assistance PDF
|
Form Name: |
Category: |
Page Count: |
File Format: |
|---|---|---|---|
|
Stelara Enrollment Form |
Patient Support Program |
04 Pages |
PDF, Fillable PDF |
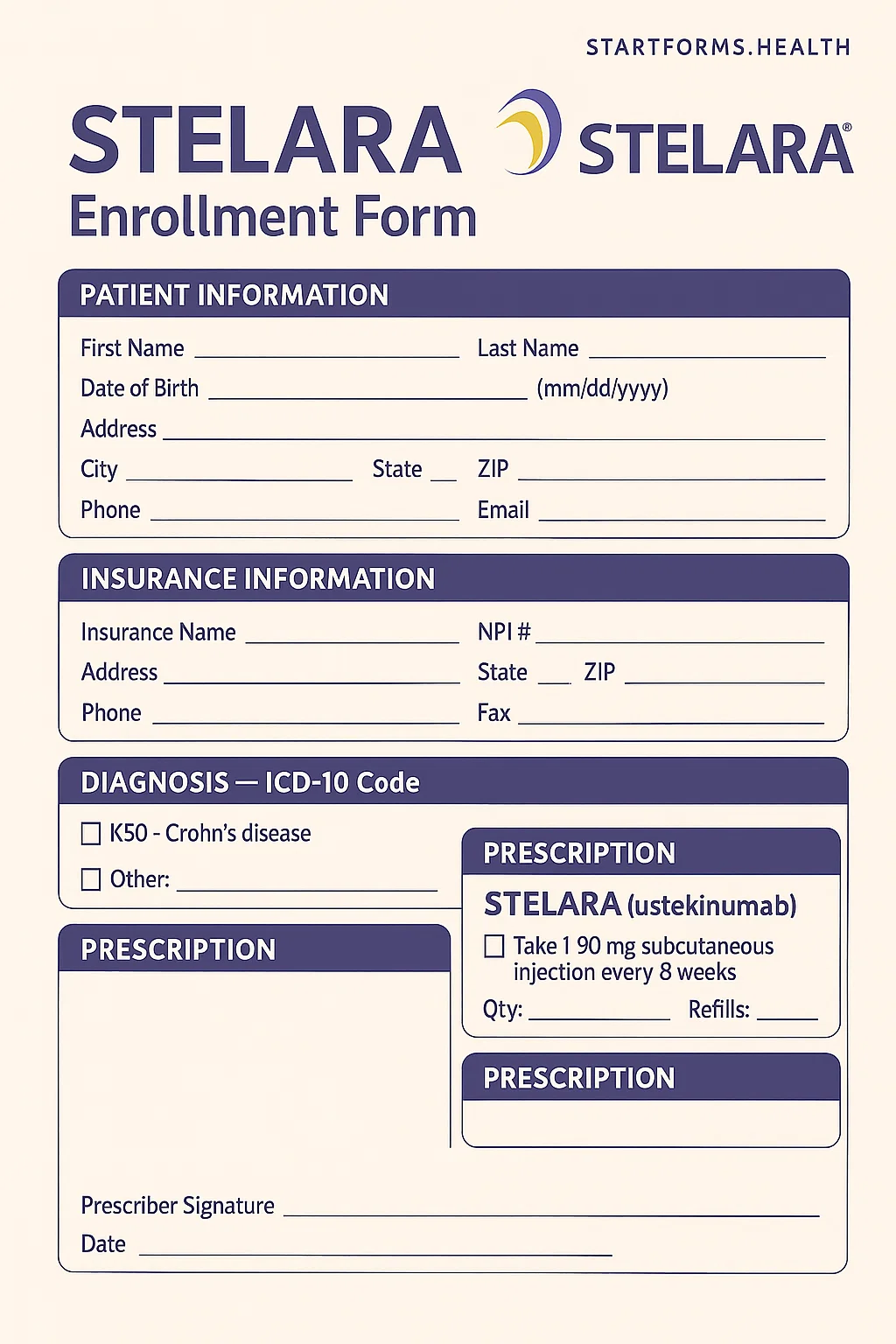
Stelara Enrollment Form
Starting treatment with Stelara requires accurate documentation to ensure insurance coverage, timely support, financial support, and access to assistance programs. The Stelara enrollment form collects required patient, prescriber, and insurance information in one document, making the process simple and more efficient. By submitting the form, patients can benefit from access to prior authorization, benefit investigation, affordability programs, and dedicated nurse navigator outreach. Download and fill out the form today to get personalized support and avoid unnecessary delays.
Form Preview
Benefits of The Stelara Enrollment Form
Delay and Denial Assistance
The Stelara enrollment form allows patients to access Jansen’s Delay and Denial Support Program. Eligible commercially insured patients can receive a Stelara if there is any delay or denial in coverage. This helps patients start their treatment on time without interruption.
Patient Assistance Program (PAP) Access
The form lets patients facing financial issues enroll in the Janssen Patient Assistance Program. The eligible patient can receive Stelara free of cost up to one year.
Copay Options
The form lets eligible patients connect with financial assistance resources, exception requests, and appeal support to help reduce out-of-pocket costs.
Key Sections of The Stelara Patient Enrollment Form PDF
1- Patient Details
The first section of the form contains all required patient information, including their name, address, gender, date of birth, and contact details.
2- Insurance Section
This section includes insurance information, such as insurer information, cardholder information, PCN number, policy number, and other details.
3- Clinical Information
It includes appropriate ICD-10 diagnosis codes, date of diagnosis, and prior treatment history.
4- Prescriber Information
It collects the prescriber’s name, practice information, office contact, signature, etc.
5- Prescription Section
It indicates induction dosing and maintenance dosing, allowing prescribers to choose a preferred specialty pharmacy or infusion center.
6- Benefits Investigation Authorization
This section ensures that the prescriber is requesting Janssen to verify insurance coverage and reimbursement options.
7- Patient Consent & Authorization
It grants Janssen permission to access and share patients’ information, enabling the activation of most support services.
How To Complete The Stelara With Me Enrollment Form?
Patient Information: Provide the patient’s full name, date of birth, gender, address, city, state, ZIP code, phone number, and email address.
Insurance Information: Attach front and back copies of the insurance cards. Also, fill in the medical insurance name, policy number, group number, cardholder name, pharmacy insurance, and PCN number.
Clinical Details: Specify the appropriate diagnosis codes, including date of diagnosis, date of previous TB test, and prior medication (if any).
Prescriber Information: Provide the prescriber’s name, office contact details, practice name, complete address, tax ID number, and NPI number.
Prescription Information: Specify the patient’s weight, date of infusion, induction dose, etc. Also, indicate pharmacy or infusion center preferences.
Prescriber Signature: The prescriber must sign and date the form to validate the prescription.
Patient Authorization: The patient or their legal representative must sign and date the HIPAA-compliant authorization section. This section is necessary to receive Nurse Navigator outreach and more support programs, such as Stelara copay assistance, discount card, savings program, etc.
Download Stelara Enrollment Form PDF
Choose your preferred format and download instantly
Frequently Asked Questions
What is the purpose of the Stelara patient enrollment form?
This form is designed to collect all required information related to the patient, prescriber, and insurance, and is used to initiate support services offered by Janssen CarePath and Stelara WithMe. Additionally, it helps in verifying benefits, assists with prior authorization, coordinates prescription services, and connects patients with available assistance programs.
Is the patient authorization mandatory?
The treatment can proceed without the patient’s authorization. But they cannot access most support services, such as Nurse Navigator outreach and affordability programs, without it.
Are Medicare or Medicaid patients eligible for copay assistance?
Not at all. Medicaid or Medicare patients are not eligible for the copay cards. But they can qualify for other support services through Patient Assistance Programs.
Where should the completed form be sent?
The completed form should be faxed or mailed to the Janssen CarPath program using the details mentioned on the form.
Can I still receive medication if my insurance denies coverage?
Of course, the eligible commercially insured patients can still receive Stelara temporarily at no cost through the Delay and Denial Assistance program.
Related Forms
Enroll in Tremfya therapy for plaque psoriasis and psoriatic arthritis with patient support and financial aid.
Fill Humira Enrollment Form to access AbbVie’s Humira Complete program for the treatment of rheumatoid arthritis, psoriasis, Crohn’s disease, and other autoimmune conditions.
