Eylea Enrollment Form – Patient & Provider Application PDF
|
Form Name: |
Category: |
Page Count: |
File Format: |
|---|---|---|---|
|
Eylea Enrollment Form |
Patient Support Program |
03 Pages |
PDF, Fillable PDF |
Eylea Enrollment Form
The Eylea enrollment form is an official application used to enroll patients in the Eylea4U support program for EYLEA treatment. It helps patients and healthcare providers access insurance verification, prior authorization, copay assistance, and patient assistance services when applicable. Completing the form accurately supports timely treatment decisions and helps prevent delays caused by insurance or documentation issues. Complete it online or download and submit it today to start treatment support without interruptions.
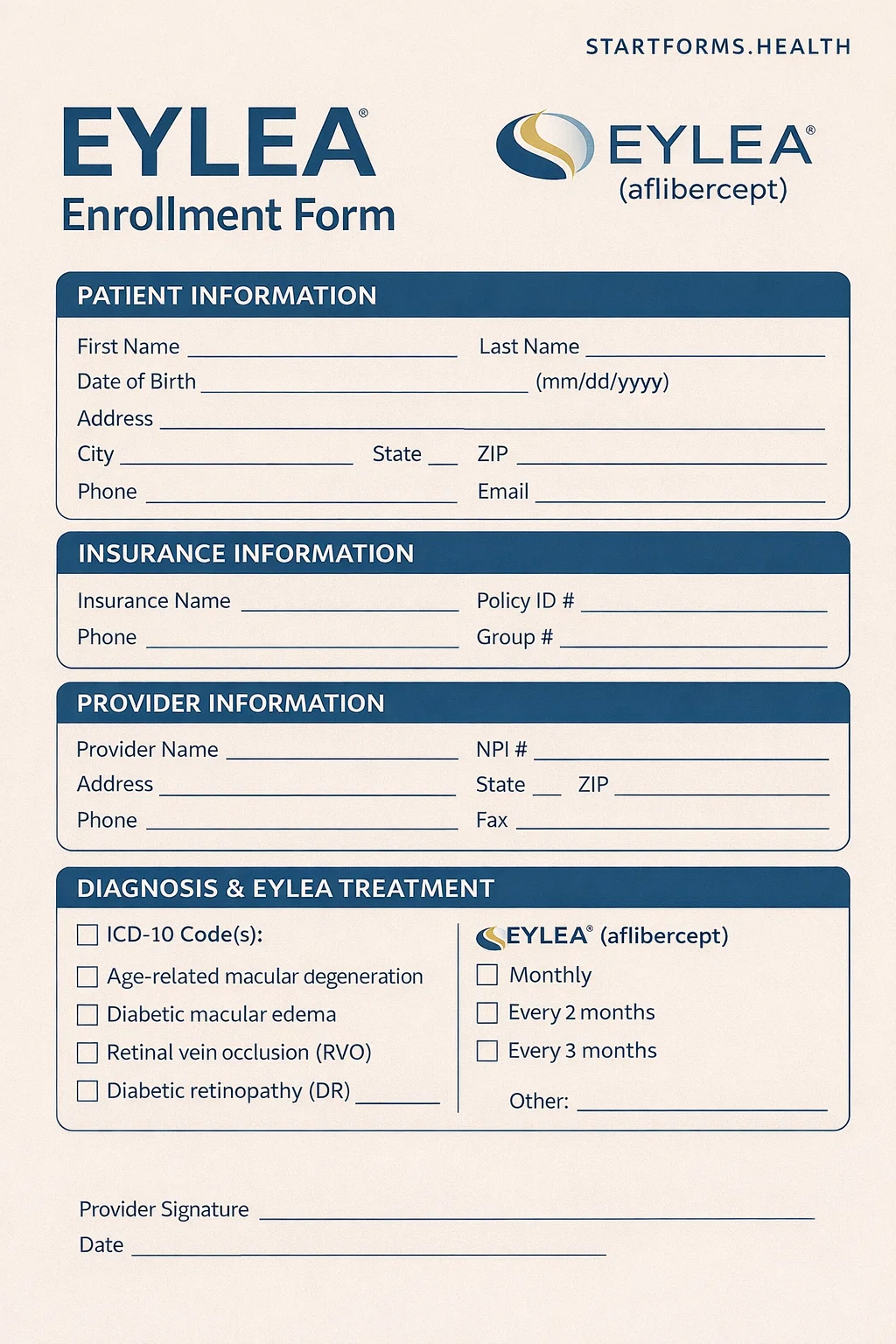
Form Preview
Benefits of The Eylea Patient Enrollment Form
Access the EYLEA4U Patient Support Program
By submitting the Eylea patient enrollment form, patients get access to EYLEA4U, which offers personalized support throughout the treatment process. This includes insurance navigation, benefit verification, and assistance services.
Claims & Appeals Support
If an insurance claim is denied, the form allows support teams to assist with claim corrections and appeal submissions, helping patients continue treatment without unnecessary interruption.
Patient Assistance Program for Uninsured Patients
Uninsured or financially eligible patients may receive medication support through PAP. The form collects required income and insurance details to assess eligibility properly.
Key Sections of The Eylea 4 u Enrollment Form
Support Requested
The first section of the form allows selection of services, such as:
- Benefits investigation
- Prior authorization services
- Co-pay assistance
- Patient Assistance Program (PAP)
- Claim and appeals support
Patient Information
This section includes the patient’s name, gender, DOB, address, email address, and contact details.
Insurance Information
It describes insurance information, including insurer, policy number, insured name, employer, group number, and phone number.
Diagnosis Details
Records the diagnosis, affected eyes, and visual acuity.
Prescription Details
It specifies Eylea dosage, refills, schedule, number of vials, allergies, specialty pharmacy preference, and shipping details.
Prescribing Physician & Office Information
It includes credentials, NPI, DEA, practice details, and office contact information. Physician certification confirms accuracy and proper use of medication.
Patient Authorization & Financial Information
Patient authorizes the use of their health information for support services and provides household income details when applying for copay or patient assistance programs.
How to Complete The Eylea Enrollment Form?
Select Support Services: Check all applicable boxes under “Support Requested” to ensure you receive the full range of assistance, such as Benefits investigation, appeals support, co-pay assistance, claim assistance, or prior authorization assistance.
Patient Information: Fill in the patient’s details, including full name, SSN, date of birth, gender, complete address, and contact details.
Patient Insurance Information: Provide the primary & secondary insurance information (if applicable), including name, insured name, employer, policy number, group number, and phone number. Indicate if the patient is uninsured.
Diagnosis/Treatment: The healthcare provider must complete the diagnosis, affected eyes, and visual acuity values accurately.
Prescription: The prescribing physician selects the appropriate EYLEA dosage schedule, number of vials, refills, and pharmacy details. Also, check the box “Yes/No” if the patient has any known allergies.
Prescribing Physician Information: Indicate the site of service, practice or facility name, physician name, specialty, state license number, complete address, and office contact details.
Signatures and Submission: Patient and physician must sign and date where required. Submit the complete form via fax or retain it on file if submitted through the e-portal.
Download Eylea 4 u Enrollment Form PDF
Choose your preferred format and download instantly
Frequently Asked Questions
What is the Eylea enrollment form?
It is used to enroll patients in the Eylea support program, helping patients receive insurance verification, prior authorization support, co-pay assistance, prescription coordination, and patient assistance for Eylea therapy.
Is the form required for every Eylea patient?
The form itself is not required for treatment, but it is recommended for patients who are seeking insurance support, financial assistance, or help with prior authorization and reimbursement.
Can uninsured patients apply using this form?
Of course, uninsured patients may qualify for the Patient Assistance Program after completing the financial information section.
Where should the completed form be submitted?
The form can be submitted by fax to the number listed on the form or retained by the healthcare provider if submitted through the official e-Portal.
Can I submit this form to the specialty pharmacy?
Yes. If required, the form allows the prescription to be forwarded to a specialty pharmacy selected by the provider or patient.
