Entyvio Enrollment Form PDF – Free Patient Application
|
Form Name: |
Category: |
Page Count: |
File Format: |
|---|---|---|---|
|
Entyvio Enrollment Form |
Patient Support Program |
08 Pages |
PDF, Fillable PDF |
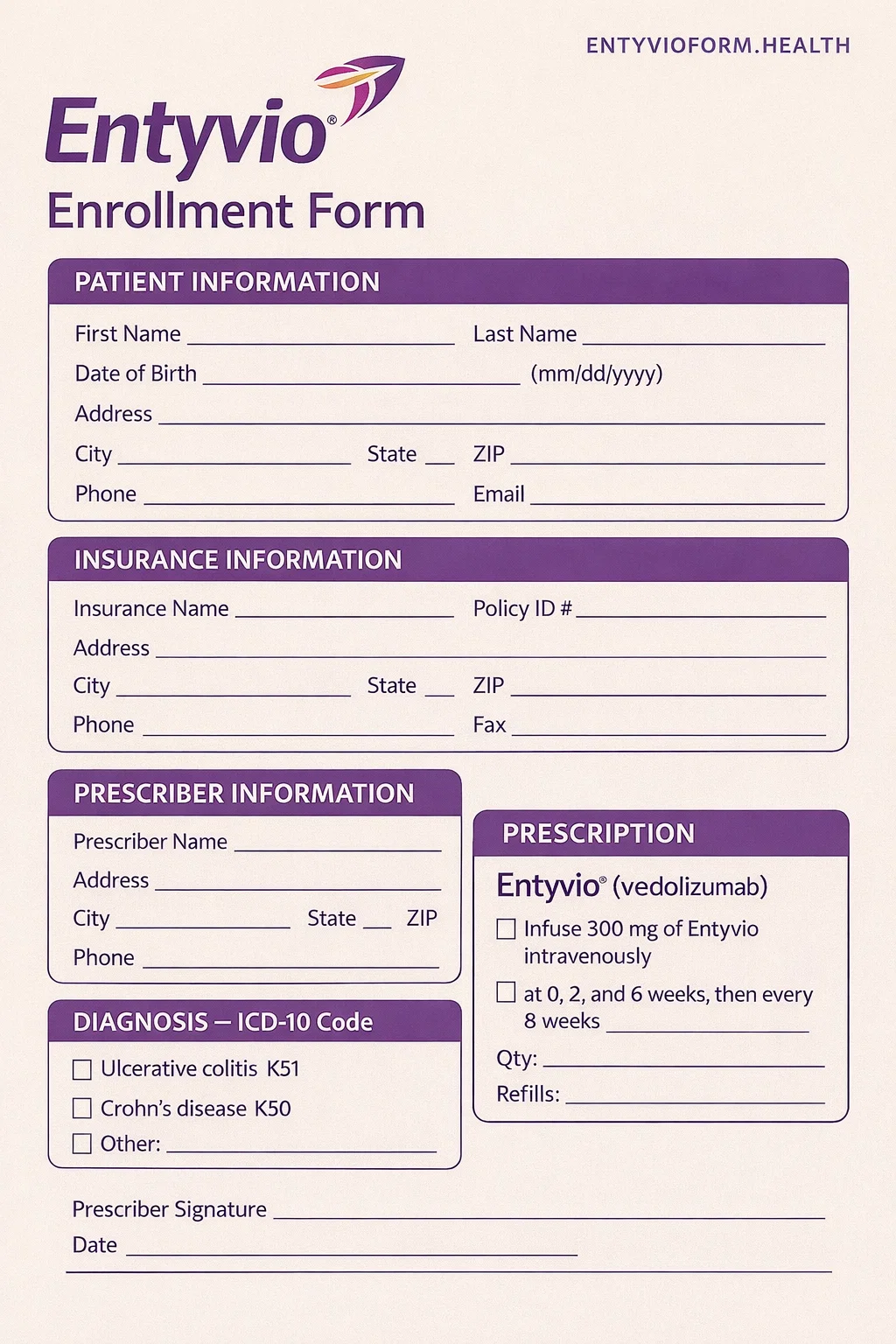
Entyvio Enrollment Form
It is an official document used to enroll eligible patients in the EntyvioConnect Patient Support Program. This form allows patients and healthcare providers to initiate Entyvio treatment while accessing insurance verification, specialty pharmacy coordination, co-pay assistance, nurse support, and educational services. Completing the form accurately helps prevent treatment delays and ensure timely access to prescribed therapy. Fill out the Entyvio enrollment form online now to start the enrollment process quickly and securely.
Form Preview
Benefits of The Entyvio Enrollment Form
Bridge Program for Coverage Gaps
Patients already on therapy who temporarily lose insurance coverage may receive continuity of care through the bridge program.
Start Program Support
Eligible new-to-therapy patients who experience insurance denial or program exclusion may receive Entyvio at no cost for a limited period through the Statt Program.
Insurance Benefit Verification
EntyvioConnect reviews the submitted insurance information to identify coverage, prior authorization requirements, and reimbursement pathways.
Key Sections of The Entyvio Enrollment Form
Patient Information
This section collects the patient’s name, contact details, address, date of birth, email address, and legal representative information (if applicable).
Insurance Section
It includes primary and secondary insurance details, including plan name, policy ID, group number, subscriber information, and prescription insurance details.
Prescriber Details
This section provides healthcare provider details, such as prescriber name, practice address, NPI number, tax ID, license number, and office contact information.
Infusion Site Information
If the infusion location is different from the prescriber’s office, this section records infusion site details, including site type, address, and provider identifiers.
Patient Clinical Information
The prescriber provides ICD-10 diagnosis codes, current medication, and known medication allergies.
Dosage and Direction for Use
It specifies whether the patient will receive Entyvio IV infusion or Entyvio Pen subcutaneous injection.
How to Complete the EntyvioConnect Enrollment Form?
Patient Information: Fill in the patient details, including their full name, complete home address, birth date, gender, phone number, and legal representative details.
Insurance Information: Provide medical and prescription coverage details, such as insurance plan, plan phone number, subscriber name, date of birth, relationship to patient, policy ID, group ID, BIN, and PCN.
Prescriber Information: Write the prescriber’s name, practice/facility name, address, office contact name, office phone number, NPI, tax ID, state license number, etc.
Entyvio Infusion Site Information: Select the infusion site of care. Also, fill in the site provider name, address, DEA number, site tax ID, NPI, and site contact details.
Patient Clinical Details: Write the appropriate ICD-10 diagnosis code, current medication, and any known medication allergies.
HIPAA and Support Program: The patient or their legal representative must sign to authorize participation and optional services.
Dosage and Direction of Use: The prescriber should select the appropriate initiation and maintenance dosing schedules.
Submit: Fax completed form to the EntyvioConnect fax number given on the form.
Download Entyvio Enrollment Form PDF
Choose your preferred format and download instantly
Frequently Asked Questions
What is the Entyvio enrollment form?
It is an official document used to enroll patients into the EntyvioConnect Patient Support Program. It allows patients to access Entyvio treatment, including insurance verification, specialty pharmacy coordination, financial assistance programs, and optional nurse support.
Who needs to complete this form?
Both the patient and the prescribing healthcare provider must complete and sign the form. The provider confirms medical necessity and treatment details, while the patient authorizes program participation and information sharing.
Can I submit the form without insurance information?
Yes, but insurance information is necessary for benefit investigations, prior authorization reviews, and eligibility determinations for financial assistance programs. An incmplete insurance information may delay enrollment.
Are patients enrolled in Medicare or Medicaid eligible for co-pay assistance?
No. The patient enrolled in federal or state healthcare programs, including Medicaid and Medicare, is not eligible for the EntyvioConnect Co-Pay Program due to program regulations.
What is the EntyvioConnect claim form?
It is used to submit treatment-related claims or supporting documentation, such as Explanation of Benefits (EOB), for co-pay assistance or reimbursement processing.
