Bimzelx Enrollment Form – Free Editable PDF for Patients
|
Form Name: |
Category: |
Page Count: |
File Format: |
|---|---|---|---|
|
Bimzelx Enrollment Form |
Patient Support Program |
02 Page |
PDF, Fillable PDF |
Bimzelx Enrollment Form
Starting BIMZELX treatment requires accurate documentation and insurance verification to ensure patients receive the right support on time. The Bimzelx enrollment form is used to connect patients, prescribers, and insurers in a single document, making the process straightforward and efficient. By completing this form, patients can access the Bimzelx Navigate Support Program, including insurance verification, financial support, and personalized patient assistance. Download, fill out the PDF, and submit it to ensure uninterrupted treatment support.
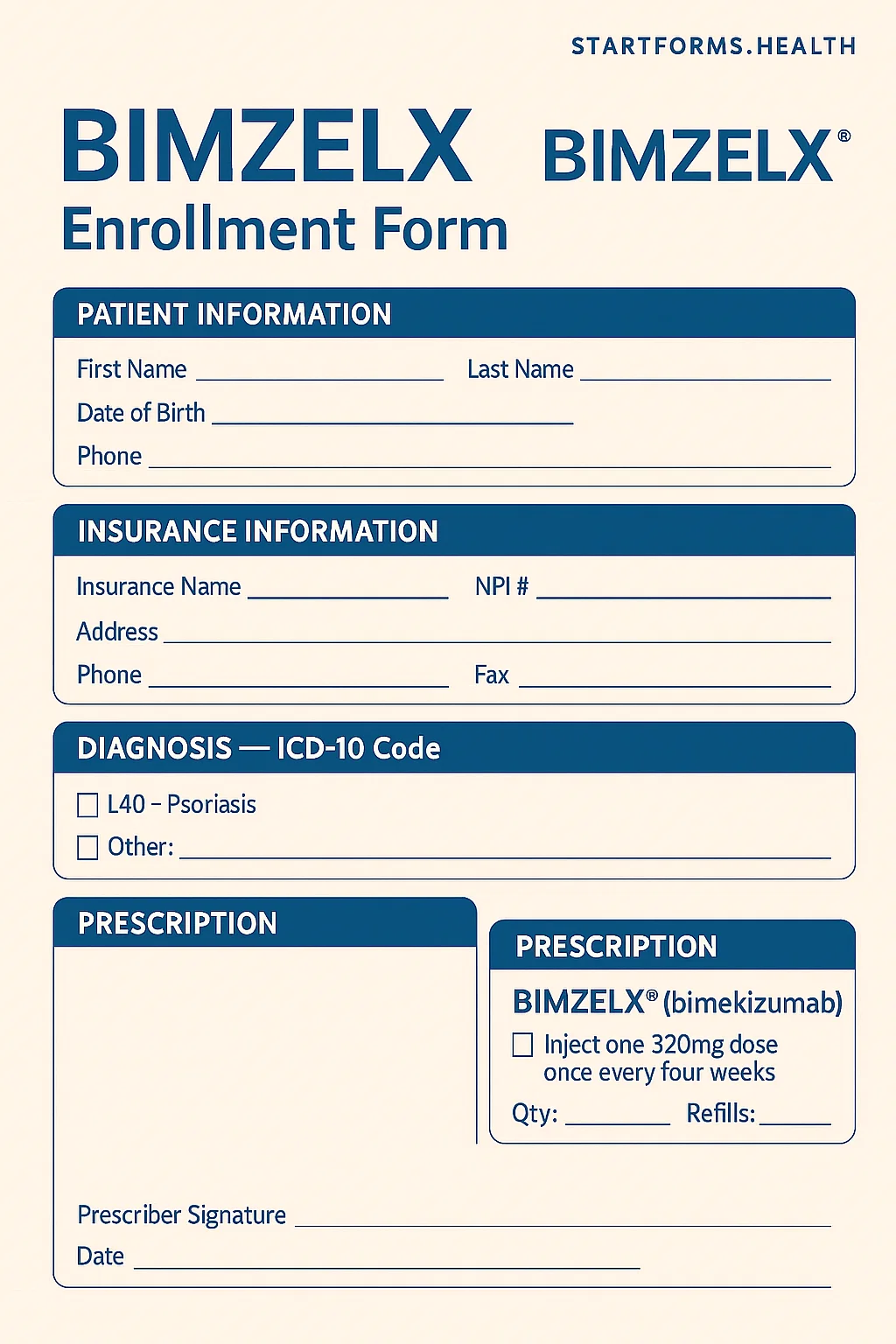
Form Preview
Advantages Of Bimzelx Enrollment Form
Access To Bridge and Saving Programs
Eligible patients may qualify for Bimzelx Navigate Bridge or Saving Programs, even if they face delays or denials in coverage. Through the Bimzelx enrollment form, the patients can receive medication at reduced out-of-pocket costs while their coverage approval is in process.
Dedicated Patient Support Services
Once enrolled, the patients get access to Bimzelx Nurse Navigators and support staff, who provide insurance assistance, treatment schedules, and medication management.
Accurate Prescription Instructions
The form has a detailed prescription instruction section, which allows prescribers to specify the exact Bimzelx product, dosage, frequency, and refill schedule. Additionally, it also ensures patients receive the exact medication in the appropriate form.
Key Sections of The Bimzelx Fillable Form
1- Patient Information
It describes the patient’s name, full address, date of birth, gender, weight, contact details, and language preference.
2- Insurance Section
This section includes medical and pharmacy details, including their tax ID, member ID, BIN, policy numbers, etc.
3- Prescriber Information
Specifies prescriber name, NPI, tax ID, license number, and office details.
4- Clinical Information Section
This section specifies the diagnosis codes, prior treatment history, and therapy notes.
5- Prescription Details
It contains medication type, dosage, frequency, and refill instructions.
How To Complete The Bimzelx Enrollment & Benefits Verification Form?
Patient Information: Provide the patient’s legal name, gender assigned at birth, date of birth, weight, street address, city, state, ZIP code, primary & alternate phone numbers, and authorized representative contact details.
Insurance Information: Attach front and back copies of the patient’s medical and pharmacy insurance cards. Also, provide the insurance details, including primary prescription insurance, prescription insurance phone number, pharmacy member ID, BIN, PCN, medical insurance ID, group number, etc.
Prescriber Information: Enter prescriber’s full name, NPI number, tax ID, office contact details, practice name, complete address, and supervising physician name.
Clinical Information: Choose the appropriate diagnosis code and list any prior treatments, intolerances, or contraindications.
Prescription Details: Select the accurate Bimzelx product, dosage, refills, and frequency based on diagnosis.
Prescriber Signature: The prescribing physician must sign and date the form to validate the prescription.
Patient Authorization: The patient or the authorized representative must sign and date the form to allow UCB to use and share their health information.
Download Bimzelx Enrollment Form PDF
Choose your preferred format and download instantly
Frequently Asked Questions
What is the purpose of the Bimzelx enrollment form?
The form is used to enroll patients in the Bimzelx Navigate programs, which include benefits verification, financial assistance, a copay card, and patient support. It collects all required patient, prescriber, and insurer information in one organized document.
Does the form include financial support options?
Of course, by submitting the form, eligible commercially insured patients can receive medication at a reduced cost through the Bridge Program while coverage is pending. On the other hand, through the savings program, patients can obtain medication for as little as $5 per dose once coverage is approved.
How long does the patient authorization remain valid?
The authorization is valid for 10 years from the date signed unless revoked earlier in writing by the patient or state law requires a shorter duration.
Related Forms
The form lets patients connect with the HeadStart Program to receive a temporary supply of OFEV until insurance or reimbursement is confirmed.
The Tremfya enrollment form streamlines the process by connecting patients and prescribers with support programs, including benefits verification, prior authorization support and affordability options.
